Researchers in Translational Neuroscience
The Department of Translational Neuroscience acts as a catalyst for enhancing bidirectional opportunities for clinical, basic and translational research in neurodegenerative diseases. The department provides the physical infrastructure and intellectual assets to conduct preclinical and translational medical research in collaboration with clinical and basic science faculty throughout MSU and strategic medical health partners in Grand Rapids.
Visit the Department of Translational Neuroscience website
Researchers
-
Jack Lipton, PhD, Department Chair
 Professor and Chair of Translational Neuroscience
Professor and Chair of Translational NeuroscienceJack Lipton and his colleagues use altered viruses to over-express some genes and silence others to determine which ones are involved in Parkinson’s disease. Using a process called high-throughput screening, he studies how various gene combinations interact to cause the survival or death of brain cells that produce dopamine, a neurochemical that declines in Parkinson’s patients. As department chair, Lipton oversees several teams studying neurodegenerative diseases.
-
Matthew Benskey, PhD
 Assistant Professor of Translational Neuroscience
Assistant Professor of Translational NeuroscienceMatthew Benskey studies the use of modified viruses, called viral vectors, to carry genetic material that could counteract Parkinson’s disease symptoms. While tremors are the most visible symptom, more than 90 percent of Parkinson’s patients also suffer gastrointestinal disorders, including constipation and difficulty swallowing. Benskey’s research has shown that the same molecular changes in the brain associated with tremors also occur in the intestinal tract.
-
Maggie Caulfield, PhD
 Assistant Professor of Translational Neuroscience
Assistant Professor of Translational NeuroscienceMaggie Caulfield focuses on the pre-clinical analysis of gene-therapy based interventions to reduce common therapeutic side effects in Parkinson’s disease. Her laboratory skill set includes cell, molecular, and histological techniques such as cell culture, flow cytometry, RNA in situ hybridization, qPCR, western blot, ELISA, immunohistochemistry, and confocal microscopy. Dr. Caulfield also spends significant time with their experimental animals performing stereotaxic surgeries, behavior ratings, and post-mortem processing.
-
Timothy Collier, PhD
 Professor of Translational Neuroscience
Professor of Translational NeuroscienceTimothy Collier, who holds the Edwin A. Brophy Endowed Chair in Central Nervous System Disorders, is a leading expert in neurodegenerative diseases, including how the normal aging of the brain predisposes patients to Parkinson’s and Alzheimer’s diseases. Part of his research is into repurposing an existing drug – an antidepressant called nortryptiline – which could be the first treatment to slow the deterioration of Parkinson’s.
-
Benjamin Combs, PhD
 Assistant Professor of Translational Neuroscience
Assistant Professor of Translational NeuroscienceBenjamin Combs studies the short circuits in the brain that cause neurological diseases, such as Alzheimer’s. Previous research has focused on a brain protein called tau, which becomes defective in Alzheimer’s patients, forming tangles and causing brain cells to die. Combs believes tau becomes toxic to brain cells before the tangles form, a finding that could lead to earlier treatments to delay or prevent Alzheimer’s.
-
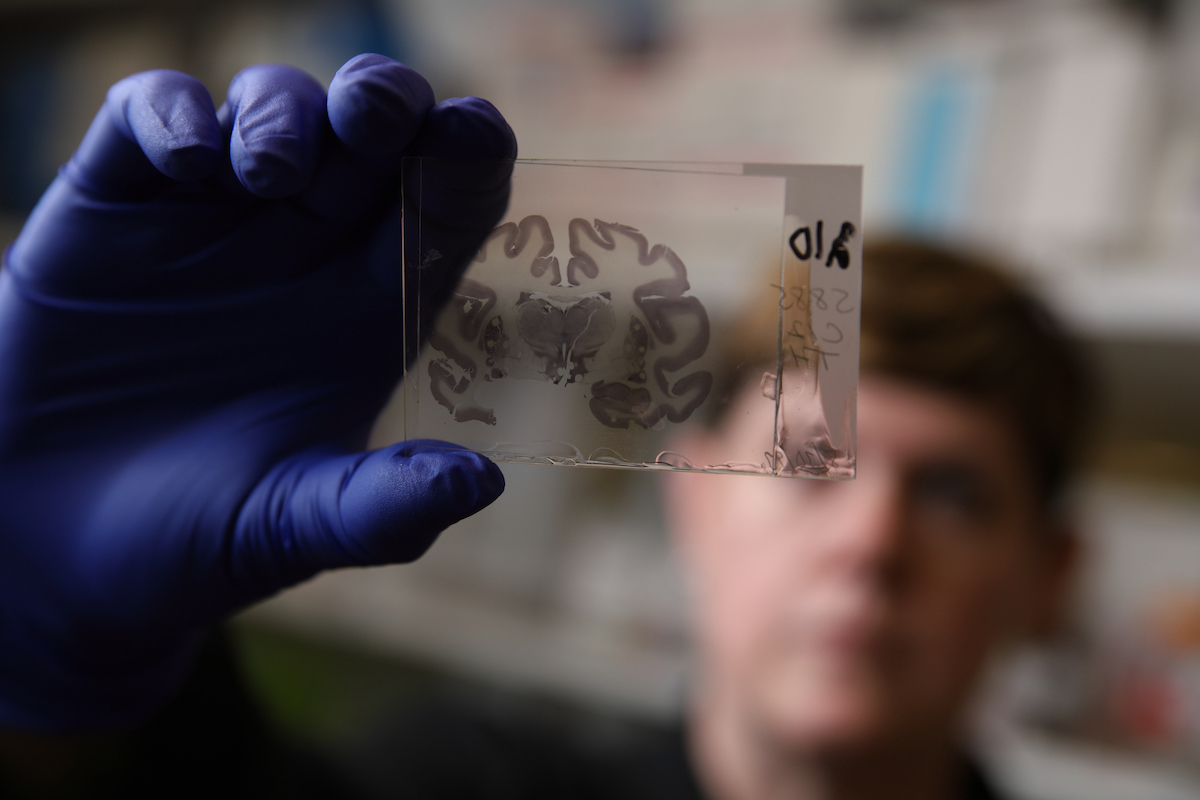
Scott Counts, PhD
 Associate Professor of Translational Neuroscience
Associate Professor of Translational NeuroscienceScott Counts is seeking new treatments to turn off molecular pathways in the brain that appear to cause Alzheimer’s disease and turn on others that appear to protect brain cells. Working with Mercy Health Saint Mary’s, Counts is heading a plan to create a repository of brain tissue samples that could provide researchers with a wealth of information about Alzheimer’s and other neurodegenerative diseases.
-
Marcia Gordon, PhD
 Professor of Translational Neuroscience
Professor of Translational NeuroscienceWhile studies have shown that two proteins in the brain – beta amyloid and tau – are associated with Alzheimer’s disease, Marcia Gordon believes an immune response and inflammation triggered by those proteins contribute to the disease. Her research has led to clinical trials of a vaccine to counter the buildup of beta amyloid, and she hopes another treatment will be developed soon to reverse the effects of tau.
-
Nicholas Kanaan, PhD
 Professor of Translational Neuroscience
Professor of Translational Neuroscience
Maibach Smiley Professor of Alzheimer’s ResearchNicholas Kanaan is developing monoclonal antibodies to hunt down and block the toxic forms of tau, a protein that appears to be a factor in many neurodegenerative diseases, including Alzheimer’s, frontotemporal dementia, traumatic brain injury and Parkinson’s. Long before symptoms appear, tau
forms into clumps and becomes toxic, causing brain cells to die. By blocking tau’s signaling pathway, Kanaan hopes to stop the death of brain cells. -
David Morgan, PhD
 MSU Foundation Professor of Translational Neuroscience
MSU Foundation Professor of Translational NeuroscienceThe key to treating Alzheimer’s disease, David Morgan believes, is in diagnosing it early and beginning treatment to prevent the onset of symptoms. As one of the country’s leading Alzheimer’s
experts, Morgan has spent his career studying the causes and looking for ways to intervene before it becomes a devastating illness. His research already has led to several clinical trials of treatments he believes could prevent full-blown Alzheimer’s. -
Joe Patterson, PhD
 Assistant Professor of Translational Neuroscience
Assistant Professor of Translational NeuroscienceJoe Patterson’s research focuses on the identification of the genetic signatures specific to the progression of synucleinopathies, such as Parkinson’s disease. An additional focus of his is the testing of potential disease modifying therapies in a synucleinopathy model that recapitulates key features of Parkinson’s disease.
-
Shreesh Sammi, PhD
 Assistant Professor of Translational Neuroscience
Assistant Professor of Translational NeuroscienceShreesh Sammi focuses on gaining insights into the mechanisms involved in neurodegenerative disorders, particularly Parkinson's disease, Amyotrophic Lateral Sclerosis, and Alzheimer's disease. He is working towards discerning the mechanism of toxicants instigated disease progression and identifying possible targets for intervention. Utilizing C. elegans and in vitro models, he has been conducting research pertaining to investigating the underlying mechanism and evaluation of the therapeutic potential of synthetic and natural compounds. He is especially interested in identifying the effects and underlying causes of Polyfluoro-alkyl substances (PFAS) associated neurotoxicity. His further interests entail studies aimed at discerning the role of Optineurin in pathologies related to Amyotrophic Lateral Sclerosis, Alzheimer's and Parkinson's disease.
-
Caryl Sortwell, PhD
 Professor of Translational Neuroscience
Professor of Translational NeuroscienceAmong her other studies, Caryl Sortwell researches why some Parkinson’s disease patients don’t respond well to levodopa, a standard treatment. The reason, she believes, is that about one-third of the patients have genetic variations that disrupt the release of a protein that helps brain neurons survive and promote the growth of new ones. Her goal is to personalize care by determining what treatment is likely to be most effective for each patient.
-
Kathy Steece-Collier, PhD
 Professor of Translational Neuroscience
Professor of Translational NeuroscienceFor some Parkinson’s patients, the side effects of the drug levodopa – including involuntary movement called dyskinesia – are as bad as the disease. Too little dopamine causes the tremors and rigid muscles characteristic of Parkinson’s, but too much dopamine, sometimes induced by the drug treatment, can cause dyskinesia. One of Kathy Steece-Collier’s research projects is aimed at improving the effectiveness of the treatment while minimizing the side effects.
-
Irving Vega, PhD
 Associate Professor of Translational Neuroscience
Associate Professor of Translational NeuroscienceIrving Vega is searching for early indicators of Alzheimer’s disease so treatment can begin before symptoms appear. Early diagnosis is critical, because neurodegeneration starts 20 or more years before clinical presentation. Vega has identified several early biomarkers that appear to be associated with Alzheimer’s and other neurological diseases, a discovery that could lead to early treatments to slow and possibly halt the disease.